An internet search using “brain injury statistics” will locate an overwhelming volume of data, most of which cite the United States Centers for Disease Control and Prevention (CDC). A representative of credible (rounded) statistics reveals (1):
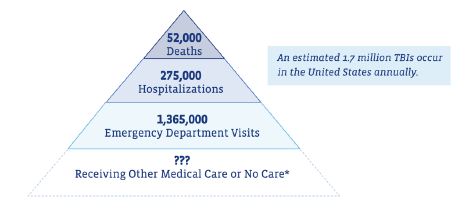
Notice that at the bottom of the pyramid, there is a large group of traumatic brain injury persons who remain uncounted. Their brain injury apparently did not warrant emergency medical services and probably would have been defined as “mild traumatic brain injury.”
Mild traumatic brain injuries are also known as concussions. It is estimated that these injuries have a prevalence of 3.8 million per year in the United States (2). Despite this high incidence, mild traumatic brain injuries and concussions are one of the least understood injuries facing the sports healthcare and the neuroscience communities today (3).
Brain injury can be categorized into two types: direct blow and inertial.
Direct blow brain injury occurs when an outside force contacts the stationary skull with enough force that the brain in affected.
Inertial brain injuries follow the universal laws of motion established by Sir Isaac Newton (1643-1727) in his 1687 book Mathematical Principles of Natural Philosophy:
- If the head is stationary and then suddenly experiences a rapid acceleration, the brain will collide with the inside of the skull. An example would be the inertial acceleration injury caused by motor vehicle collisions.
- If the head is moving and suddenly collides with an object, the brain will similarly collide with the inside of the skull. This type of brain injury is commonly seen in sports and falls.

Direct Blow
 Inertial
InertialSome brain injuries are a combination of direct blow and inertial injury.
Both direct blow and inertial mechanisms of brain injury will affect the structures of the cervical spine (neck).
The most widely accepted criteria for diagnosing traumatic brain injury are from the American Congress of Rehabilitation Medicine, which include (4):
- Any period of loss of consciousness.
- Any loss of memory for events immediately before or after the accident (posttraumatic amnesia).
- Any alteration in mental state at the time of the accident, including feeling dazed, disoriented, or confused.
- Any focal neurological deficits that may or may not be transient but that do not exceed: loss of consciousness of 30 minutes; an initial Glasgow Coma Scale (GCS) score of 13-15 (below); a Glasgow Coma Scale score of less than 13 is not graded as “mild”; posttraumatic amnesia of 24 hours.
The Glasgow Coma Scale (GCS) is a neurological scale used to give a reliable and objective assessment of the conscious state of a person, adult or child, primarily following head injury. It was published in 1974 by professors of neurosurgery at the University of Glasgow’s Institute of Neurological Sciences (5):
GCS less than 8–9
GCS 9–12
GCS 13-15
Severe Brain Injury
Moderate Brain Injury
Minor Brain Injury
- The scale is composed of three tests: eye, verbal, and motor
- A score of 15 is essentially normal, a fully awake person.
- A score of 3 indicates a deep coma.
A copy of the Glasgow Coma Scale is included at the end of this paper.
••••
In 2006, the journal Brain Injury published a study titled (6):
Is there a Relationship Between Whiplash-Associated Disorders and Concussion in Hockey?
The objective of this study was to examine the relationship between the occurrence of whiplash-associated disorders (WAD) and concussion symptoms in hockey players. It is a prospective cohort observational study. Twenty hockey teams were followed prospectively for one season. Team therapists completed acute and follow-up evaluations for all of the players who received either a whiplash mechanism injury or a concussion injury.
Important to the discussion is a review of the Quebec Task Force’s Whiplash Associate Disorders (WAD) Classification Symptoms:
0 No neck complaints
I Complaint of neck pain, stiffness, or tenderness
II Neck complaint with musculoskeletal signs
III Neck complaint, musculoskeletal signs, and neurological signs
IV Fracture and/or dislocation
An important understanding of this classification is that WAD grade 0 (no neck complaints) patients may still suffer from symptoms that are not neck symptoms, such as headache, dizziness, etc. These authors point out the symptomatic overlap between WAD neck injuries and concussion brain injuries:
| Whiplash-Associated Disorder Symptoms | Concussion Brain Injury Symptoms |
| Headache | Headache |
| Dizziness | Dizziness |
| Ringing in the ear | Ringing in the ears |
| Memory Problems | Memory Problems |
| Visual Disturbances | Visual Disturbances |
The authors note that there is a strong association between whiplash induced neck injuries and the symptoms of concussion in hockey injuries. Both the neck and the brain should be evaluated when dealing with athletes/patients suffering from either diagnosed mechanism of injury. The authors state:
- Concussions can occur from whiplash-type neck injury mechanisms.
- Neck injuries can occur from head trauma mechanisms.
The authors state:
“Participants with WAD I and WAD II can display as many concussive symptoms or even more than those experienced by participants with WAD III.”
“This study clearly demonstrates there is an association between whiplash-induced neck injuries and the symptoms of concussion.”
“It is reasonable that hockey players who experience a head/neck complex acceleration/deceleration may experience a whiplash-associated disorder.”
“As all subjects in this study displayed symptoms of both injuries, it is recommended that the athlete adequately clear both evaluations before return to play after a WAD and/or concussive injury.”
“It was observed that concussion and WAD injuries are strongly linked.”
“It is important for the clinician treating a patient or athlete for WAD to evaluate for symptoms of concussion” and to conduct a “thorough cervical evaluation when dealing with concussed players.”
It is uncommon to injure the head without injuring the neck. Likewise, it is uncommon to injure the neck without injuring the head. The symptoms of head injury and neck injury overlap. Therefore, all patients who have injured either their neck or their head should have both regions thoroughly evaluated and treated.
••••
In 2015, an important study on this topic was published in the journal The Physician and Sports Medicine, and titled (7):
The Role of the Cervical Spine in Post-concussion Syndrome
The authors note that there is considerable overlap of the signs and symptoms of mild traumatic brain injury and of whiplash neck injury. This overlap of presentation may cause confusion as to the source of symptomatology. A “wait and see” approach to management of an assumed brain injury may be completely inappropriate if in fact the symptoms are attributed to the neck. Neck derived symptoms require early and persistent interventions.
This paper reviews the existing literature surrounding the numerous proposed theories of post-concussive syndrome and introduces another potential, and very treatable, cause of this chronic condition: cervical spine dysfunction due to concomitant whiplash-type injury.
The authors also provide a comparative chart contrasting mild traumatic brain injury with whiplash neck injury:
| Signs and Symptoms of Mild Traumatic Brain Injury | Signs and Symptoms of Whiplash Injuries |
| Headache Pressure in Head |
Headache |
| Neck pain | Neck/shoulder pain Reduced/painful neck movements |
| Nausea/vomiting | Nausea/vomiting |
| Dizziness Balance problems |
Dizziness Unsteadiness |
| Blurred Vision Sensitivity to Light |
Vision problems |
| Difficulty remembering Confusion Feeling Like “In a Fog” Difficulty Concentrating |
Memory problems Problems Concentrating |
| Sensitivity to Noise | Ringing in Ears |
| Feeling Slowed Down “Don’t Feel Right” Nervous / Anxious / Irritable Sadness / More Emotional Fatigue / Low Energy /Drowsiness Trouble Falling Asleep |
Reduced/painful Jaw Movements Numbness, Tingling or Pain in Arm or Hand Numbness, Tingling or Pain in Leg or Foot Difficulty Swallowing |
The symptoms of headache and dizziness that are so prevalent in concussion-type injuries may actually be the result of neck injury mechanisms.
The authors of this article discuss the cases of 5 patients with diagnosed post-concussive syndrome. They all experienced very favorable outcomes following various treatment and rehabilitative techniques aimed at restoring cervical spine function. The treatment included chiropractic spinal manipulation.
These authors propose that a cervical injury, suffered concurrently at the time of the mild traumatic brain injury, acts as a “major symptomatic culprit in many post-concussive syndrome patients.” They state:
“Any significant blunt impact and/or acceleration/deceleration of the head will also result in some degree of inertial loading of the neck potentially resulting in strain injuries to the soft tissues and joints of the cervical spine.”
“Acceleration/deceleration of the head–neck complex of sufficient magnitude to cause mild traumatic brain injury is also likely to cause concurrent injury to the joints and soft tissues of the cervical spine.”
“[It is] well established that injury and/or dysfunction of the cervical spine can result in numerous signs and symptoms synonymous with concussion, including headaches, dizziness, as well as cognitive and visual dysfunction, making diagnosis difficult.”
The five patients diagnosed with post-concussive syndrome were treated successfully in a chiropractic clinic. Their improvement was rapid and the results were long-lasting. Their treatment included manipulation of joints that displayed restrictive segmental motion. The authors concluded:
“Management of persistent post concussive symptoms through ongoing brain rest is outdated and demonstrates limited evidence of effectiveness in these patients.”
“[Instead, there is evidence that] skilled, manual therapy- related assessment and rehabilitation of cervical spine dysfunction should be considered for chronic symptoms following concussion injuries.”
This study highlights the lack of understanding that it is essentially impossible to sustain a traumatic brain injury without also injuring the soft tissues of the cervical spine. It is anatomically and biologically probable that these cervical spine injuries cause many of the symptoms of the post-concussion syndrome.
The study showed that traditional chiropractic management of post-concussive syndrome patients resulted in rapid and sustained improvement in signs and symptoms, allowing the athlete to return to full competition.
It is recommended that all patients who are likely suffering from a mild traumatic brain injury be referred to a chiropractor for cervical spine evaluation and treatment.
It is also recommended that all patients suffering from the post-concussive syndrome (long-term sequelae to mild traumatic brain injury) should be referred to a chiropractor for cervical spine evaluation and treatment.
••••
In 2016, an article was published in the Journal of Athletic Training, titled (8):
Cervical Injury Assessments for Concussion Evaluation
The objective of this study was to provide information on clinical tests that can differentiate cervical injury from pathologic conditions of vestibular or central origin. The authors note that concussions elicit symptoms due to brain damage, whereas cervical injury triggers symptoms due to neck-tissue damage. The authors state:
“Cervical injuries and concussion can share similar mechanisms and nearly identical symptoms or causes.”
“Symptoms or causes alone may be insufficient to differentiate between patients with a concussion and patients with cervical injuries.”
“If patients exhibit dizziness, headache, or other symptoms after a collision, they are almost automatically diagnosed as having sustained a concussion. Patients with cervical injury after a pathomechanical event affecting the head or neck may manifest nearly identical symptoms.”
“Whereas concussion and cervical injury may induce almost identical symptoms, their treatment methods differ.”
“Patients who have post-concussive syndrome after sport concussion and exhibit symptoms of dizziness, neck pain and tenderness, or headaches may have cervicogenic dysfunction.”
The authors offer these common symptoms of concussion and cervicogenic injury:
| Symptom | Concussion | Cervical Injury |
| Headache | YES | YES |
| Dizziness | YES | YES |
| Tinnitus | YES | YES |
| Irritability | YES | YES |
| Chronic traumatic encephalopathy | YES | NO |
| Sleep disturbances | YES | YES |
| Blurred vision | YES | YES |
| Neck stiffness | YES | YES |
| Balance disturbances | YES | YES |
| Depression | YES | NO |
| Cognitive deficits | YES | YES |
| Memory deficits | YES | NO |
| Attention deficits | YES | YES |
| Decreased cervical range of motion | NO | YES |
| Decreased isometric neck strength | YES | YES |
The authors note that the symptoms that are caused by injury to the soft tissues in the neck will disrupt the afferent pathways that relay information from the neck to the brain. Patients with cervical injury respond immediately to soft tissue massage, passive stretching, strength training, cryotherapy, and cervical manipulation.
••••
In 2016, an article was published in the journal BMJ Open Sport & Exercise Medicine, titled (9):
Concussion with Primary Impact to the Chest and the Potential Role of Neck Tension
The objective of this study was to assess the biomechanical responses to strain in the upper cervical spine and brainstem from impact to the chest. They indicate that cranio-cervical stretch could be a factor in concussion by causing strain in the upper cervical spinal cord and brainstem.
Studies show that during maximum cervical spine flexion, there is a downward displacement of the spinal cord that causes a stretching of the spinal cord. The authors note:
“Cranio-cervical stretch resulting from tension and flexion in the upper cervical spine has been reported to be an important factor in concussion.”
“Strains in the upper spinal cord and brainstem are important factors in concussion.”
“Neck tension or strain along the axis of the upper cervical spinal cord and brainstem is a possible mechanism of brain injury.”
This study is quite important for chiropractors as it suggests that head-neck flexion-tractional inertial injuries to the brainstem and upper cervical spinal cord, result in the concussion syndrome. In such cases, management of the cervical spine may greatly improve clinical outcomes.
••••
In 2022, a study was published in the journal Musculoskeletal Science and Practice, titled (10):
Cervical Musculoskeletal and Sensorimotor Impairments 4 weeks to 6 Months Following Mild Traumatic Brain Injury:
The objective of this study was to determine whether cervical impairments impair the expected recovery times following concussions. It is an observational cohort study using 72 individuals, 4 weeks to 6 months post mild traumatic brain injury (mTBI), of which 35 were asymptomatic, and 37 were symptomatic. The authors state:
“Neck pain and disability has been reported both acutely and sub-acutely following mild Traumatic Brain Injury (mTBI) supporting the proposition of potential cervical spine involvement in mTBI.”
“Cervical musculoskeletal and/or cervical sensorimotor impairments may underlie these persistent symptoms post mTBI.”
“[The] forces occurring during a mTBI are far more than those considered necessary for a neck injury.”
These authors note:
“Individuals post-mTBI also report symptoms other than neck pain that have been shown to be associated with cervical impairments in painful neck disorders (traumatic and non-traumatic) such as headache, dizziness, unsteadiness, and visual symptoms.”
“Findings from this study support the potential presence of persistent cervical musculoskeletal and/or cervical related sensorimotor impairments among some adults 4 weeks to 6 months following mTBI especially in those with persistent symptoms.”
“Overall findings lend further support to clinical recommendations for cervical spine assessment following mTBI especially in those with persistent symptoms.”
“These findings support prior recommendations for cervical spine screening post-mTBI regardless of symptom status.”
“Cervical spine assessment in those with persistent symptoms post-mTBI is now recommended.”
••••
Earlier this year (2023), a study was published in the Journal of Head Trauma Rehabilitation, titled (11):
Neck Symptoms and Associated Clinical Outcomes in Patients Following Concussion
The objective of this study was to examine the frequency and association of neck pain symptoms in patients with a concussion. It assessed 331 patients aged 9 to 68 years with a diagnosed concussion, 1 to 384 days post-injury (38% female, 62% male).
Neck symptoms have been gaining attention in the concussion population, with some authors advocating for the description of cervical spine disorder as a clinical profile of patients with concussions. The authors state:
“Concussions are frequently associated with violent movements in the head and neck, leading to whiplash-associated injury and neck pain.”
“Neck pain and stiffness symptoms are common in patients with a concussion following high-energy mechanisms of injury including MVCs or falls from height.”
“It is vital to recognize concussion-related neck pain as a highly prevalent cause of disability and a significant economic burden within the general population.”
“Providers should evaluate neck symptoms and consider targeted treatment strategies to limit their effects in patients with a concussion.”
“The clinical associations of concussions with severe neck symptoms presented in this study are supported by previously described associations in the whiplash literature.”
This article adds to the recommendation that all patients with traumatic brain injury be referred to a chiropractor for neck assessment and management.
REFERENCES:
- https://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf Accessed May 18, 2023.
- Langlois JA, Rutland-Brown W, Wald MM; The Epidemiology and Impact of Traumatic Brain Injury: A Brief Overview; Journal of Head Trauma Rehabilitation; September-October 2006; Vol. 21; No. 5; pp. 375–378.
- Thompson J, Sebastianelli W, Slobounov S; EEG and Postural Correlates of Mild Traumatic Brain Injury in Athletes; Neuroscience Letters; April 4, 2005; Vol. 377; No. 5; pp. 158–163.
- Kay T, Harrington DE, Adams R, et. al; Definition of Mild Traumatic Brain Injury; Journal of Head Trauma and Rehabilitation; 1993; Vol. 8; No. 3; pp. 86-87.
- Teasdale G, Jennett B; Assessment of Coma and Impaired Consciousness: A Practical Scale; Lancet; July 13, 1974; Vol. 304; No. 7872; pp. 81-84.
- Hynes LM, Dickey JP; Is there a Relationship Between Whiplash-Associated Disorders and Concussion in Hockey?; Brain Injury; February 2006; Vol. 20; No. 2; pp. 179-188.
- Marshall CM, Vernon H, Leddy JJ, Baldwin BA; The Role of the Cervical Spine in Post-concussion Syndrome; The Physician and Sportsmedicine; July 2015; Vol. 43; No. 3; pp. 274-284.
- Cheever K, Kawata K, Tierney, Galgon A; Cervical Injury Assessments for Concussion Evaluation; Journal of Athletic Training; December 2016; Vol. 51; No. 12; pp. 1037–1044.
- Jadischke R, Viano DC, McCarthy J, King AI; Concussion with Primary Impact to the Chest and the Potential Role of Neck Tension; BMJ Open Sport & Exercise Medicine; October 16, 2018; Vol.4; No. 1; pp. e000362.
- Galea O, O’Leary S, Treleaven J; Cervical Musculoskeletal and Sensorimotor Impairments 4 weeks to 6 Months Following Mild Traumatic Brain Injury: An Observational Cohort Study; Musculoskeletal Science and Practice; February 2022; Vol. 57; Article 102490.
- Oyekan AA, Eagle S, Trbovich AM, Shaw JD, Schneider M, Collins M, Lee JY, Kontos AP; Neck Symptoms and Associated Clinical Outcomes in Patients Following Concussion; Journal of Head Trauma Rehabilitation; February 28, 2023 [epub].
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”